Professor Chris O’Brien (1969)
Professor Chris O’Brien (School Captain 1969)
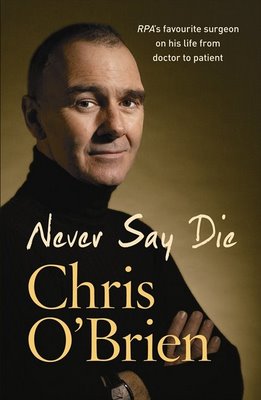
In 2009, Parramatta Marist lost one of its most illustrious old boys, Professor Chris O’Brien. A man who dedicated his life serving the needs of others. before his death he visited Parramatta Marist and spoke to the current student body. See PDF from the Parramatta Advertiser for the story: Prof. O’Brien Visit
If you wish to make a donation to the Chris O’Brien Cancer Centre please click on this link: Lifehouse at RPA
Chris O’Brien graduated in medicine from the University of Sydney in 1976 and then completed his residency and surgical training at Royal Prince Alfred Hospital. He decided to specialise in head and neck surgery and undertook clinical fellowships in that discipline in England and the USA, returning to Australia in 1987 to join the staff of RPAH as a consultant head and neck surgeon. There he contributed to the expansion of the clinical service and also established a comprehensive head and neck database which is now the largest in Australasia and one of the largest in the world.
He also established a basic research program and an international fellowship program under the umbrella of the Sydney Head and Neck Cancer Institute which he founded in 2002.
Professor O’Brien had two postgraduate degrees from the University of Sydney – a Masters of Surgery for basic research in microvascular surgery and a Doctorate in Medicine for his work on the management of metastatic cancer in the neck.
He was the author of over one hundred scientific papers and 17 book chapters and he has been honoured with invitations to many countries and institutions as a visiting professor and guest lecturer, including invitations to give numerous prestigious named lectures including the Hayes Martin Lecture in Washington in 2004, the Eugene Myers International Lecture in Los Angeles 2005, the inaugural Jatin P Shah Lecture in Prague2006 and the Semon Lecture in London 2006. He was also made an Honorary Fellow of the Royal College of Surgeons of England in recognition of his contribution to the training of young British surgeons.
In 1998 he founded the Australian and New Zealand Head and Neck Society was president in 2004. The Society continues to flourish. The Society also offers The Chris O’Brien Travelling Fellowship.

He was also a member of the American Head and Neck Society and was the first non-American to be invited to join its Council.
In 2003 Professor O’Brien became Director of the Sydney Cancer Centre, based at Royal Prince Alfred Hospital and the University of Sydney, while maintaining all of his clinical, teaching and research responsibilities. Over recent years he developed a proposal to transform the Sydney Cancer Centre into a comprehensive cancer centre and that project is moving forward with great momentum.
Chris O’Brien was widely known to the people of Australia for his many appearances over the last 12 years on the reality TV program RPA and on Australia Day 2005 he was made a Member the Order of Australia (AM) for his services to medicine. He was a devoted husband and father with many interests including running, skiing, reading and playing guitar.
Unfortunately, in November 2006 he was diagnosed with a malignant brain tumour necessitating three operations, radiotherapy and months of chemotherapy. He stepped down from all of his clinical and administrative positions at the time of his diagnosis in order to concentrate on his recovery.
Professor O’Brien died at Sydney’s Royal Prince Alfred Hospital on Thursday June 4 2009, losing his three-year battle with brain cancer.
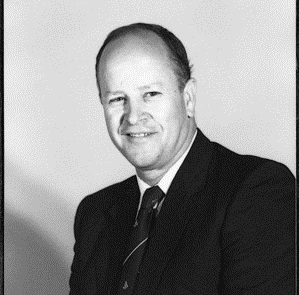
Professor Len Harrison
Len Harrison MB BS (UNSW), MD (UMelb), DSc (UMelb), FRACP, FRCPA is (2012) a Professor in the Department of Human Biology, University of Melbourne, and Head, Autoimmunity and Transplantation Division, Walter and Eliza Hall Institute of Medical Research, and Burnet Clinical Research Unit, Royal Melbourne Hospital (RMH). He was Director of the Department of Clinical Immunology, RMH, from 1987-2009. Prior to post-doctoral research at the NIH on a C.J. Martin Fellowship, he worked with Roger Melick and FIR (‘Skip’) Martin. On returning to Melbourne he was Endocrinologist and Head of the Endocrine Lab at RMH until his current (2012) appointments in 1987. His research is focused on the pathogenesis and prevention of diabetes. Len is an author on over 480 research publications and several books.
His awards for research include the Wellcome (Glaxo) Australia Medal, Susman Prize from the RACP, Kellion Medal from the ADS and Rumbough Award from the Juvenile Diabetes Research Foundation (JDRF) International. He has served on NHMRC Medical Research Committee and the Health Research Ethics Committee, been a Director of the Australian Society for Medical Research, Secretary and President of the Australian Diabetes Society, Chairman of the Scientific Review Committee of the JDRF, member of the JDRF Research Advisory Board, President of the Immunology of Diabetes Society, and is a Center Director, Trialnet International.
He and his team at the Walter and Eliza Hall Institute of Medical Research study mechanisms of immune regulation in health and disease, in particular antigen-specific regulatory T cells and antigen-specific immunotherapy. Our research is directed towards the prevention of diabetes, a major public and personal health problem that in developed countries directly accounts for 10% of health expenditure. They are currently (2012) undertaking clinical trials for a Type1 Diabetes vaccine.
Source: Australian Diabetes Society and Walter & Eliza Hall Institute of Medical Research
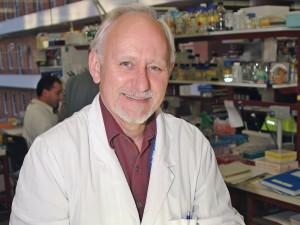
Associate Professor Raoul Walsh (1968)
Raoul completed his Higher School Certificate in 1968. He went on to a science degree at Macquarie University. A career in the health service led Raoul to a PhD at Newcastle University in 1995, where he continues (2012) as an Associate Professor in the School of Medicine and Public Health. his research was “smoking and its effect on pregnancy”.
Raoul Walsh is (2012) also a part-time Senior Research Academic with the Centre for Health Research & Psycho-oncology (CHeRP). Associate Professor Walsh’s role with the Cancer Council includes contributions to policy development and intervention research across a wide range of smoking-related issues.
Prior to Prof. Walsh’s academic appointment he obtained extensive experience in public health administration and program evaluation, initially as Team Leader of the Hunter Drug Advisory Service and then as Coordinator of Drug and Alcohol Services for the Hunter Area Health Service.
His PhD on smoking cessation in pregnancy resulted in a number of key publications which have been widely cited. Prof. Walsh was principal investigator on a National Health and Medical Research Council grant which initiated the largest evaluation of antenatal smoking dissemination methods ever undertaken in Australia. He has published widely on the subject of substance abuse with a total of over 50 papers in refereed journals. In 2001, he was first author of a behavioural science learning module on smoking cessation commissioned by the World Health Organisation.
Prof. Walsh and his colleagues were the first to demonstrate convincingly that usual care doctors and midwives, not just behavioural specialists, were capable of significantly increasing quit rates in pregnant women when a systematic program was adopted. His other research on smoking in pregnancy includes reviews of the health effects and of the effectiveness of interventions, as well as studies examining the validity of smoking self-report in pregnancy and documenting the attitudes of pregnant women and of antenatal clinic staff to this problematic issue.”
He has also conducted research evidencing public support for tobacco plain packaging.
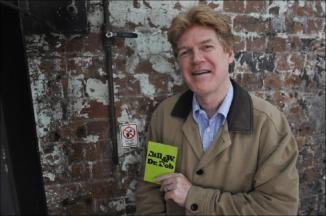
Clinical Associate Professor Stephen Jurd (1971)
Stephen completed his Higher School Certificate in 1971. He went on to complete a medical degree and a fellowship in psychiatry. He had a special interest in additions which led him to become a Clinical Associate Professor in Addiction Medicine at Sydney University (based at Royal North Shore Hospital). His research interests include using Alcoholics Anonymous to help patients. This extended to producing a play in 2011 “Bill W. and Dr. Bob” at the Carriage Works theatre Everleigh Sydney. The play is about the founders of Alcoholics Anonymous. He is also (2012) Director of Training in Psychiatry at Northern Sydney Central Coast Health.
He developed the Drug and Alcohol Services at Royal North Shore Hospital from 1984 to 2006. He initiated Phoenix Unit, a prominent Minnesota model rehab which he directed for 14 years. He chaired the Section on Alcohol and Other Drugs for six years and was the inaugural chair of the Subcommittee for Advanced Training in Addiction Psychiatry. Since 2006 he has been Director of Postgraduate Training in Psychiatry in northern Sydney. He was chair of the RANZCP Committee for Training from 2008 to 2014. He has published 30 scientific papers, participated in the development of clinical guidelines and has presented at national and international meetings. He has been granted the title of Clinical Associate Professor at the University of Sydney.
Source: The Sydney Retreat
Professor Michael Gracey AO
Michael graduated from Sydney University and specialised in paediatrics. He has worked with Australian Aboriginal children and their families and communities, particularly in remote areas in the north and central parts of Western Australia, for more than 35 years. He has worked with other ethnic groups, including Tibetans, Papua New Guinean people, Indonesians, Thais and Indians. His long interest in international child health led to his appointment as President of the International Paediatric Association. This involved work with international organisations including WHO and UNICEF in many countries and on all inhabited continents.
He was for many years the Principal Medical Adviser on Aboriginal Health to the Government of Western Australia. In 1997 he was made Australia’s first Professor of Aboriginal Health at Curtin University in Perth.
For many years he has had a strong professional interest in the interactions of nutrition and infection and their impacts on growth of infants and children. He is currently (2012) Medical Adviser to the Unity of First People of Australia, an Aboriginal driven, community-based, not-for-profit organisation.
He was made an Officer of the Order of Australia (AO) in 2001.
Source: Sydney University Medical School
Sadly, Michael passed away on 22 April 2021.
Professor Michael Gracey AO, an Old Boy from the illustrious Class of 1955, in 2014 emailed Adam Hendry, President of the Old Boys Union, and was interested to hear of his old school’s recent achievements:
“I was interested to learn of my old school’s international outreach – well done. I was also interested in …. problem-based learning. Not surprisingly, much of my training, particularly in the clinical parts of my education, was just that. But it wasn’t called PBL in those days.”

Very high praise indeed when you get a snapshot of Professor Gracey’s achievements:
“I studied Medicine at Sydney Uni, graduating at the end of 1961. I worked in Sydney (RPAH), Melbourne (Royal Children’s Hospital), the then Territory of Papua New Guinea, then in the UK for 2 years before moving to Perth in 1970 working as a paediatrician at the Children’s Hospital there for almost 20 years. While I was there I developed a collaboration with the Paediatric Department of the University of Indonesia (Jakarta) and with other Indonesian hospitals and clinics. While I was in WA, I became the Principal Medical Adviser on Aboriginal Health to the WA Dept of Health. In 1997, I was made Professor of Aboriginal Health at Curtin University (Perth) – the first such appointment in Australia. In the 1970s and 80s I worked in other countries, mostly in the Asia-Pacific Region including India, Singapore and Thailand and with Tibetan refugees in the Himalayas; while I was there (Dharamsala, north India), I had a private audience with his Holiness the Fourteenth Dalai Lama.
I have worked with remote, very remote, rural and urban Aboriginal people, mostly in WA for more than 45 years and continue this in my “retirement”.
I worked with the International Paediatric Association (IPA) for many years; the IPA represents about 600,000 thousand paediatricians in more than 100 countries. I was the first Australian to be made President of the IPA and, as part of my responsibilities, visited dozens of countries on all inhabited continents; many of these are among the world’s poorest nations.
In my retirement I teach young Vietnamese doctors and nurses at hospitals in Hanoi ….. I am an Honoured Professor in the Kazakh National Medical university in Almaty, Republic of Kazakhstan and that I was made an Officer of the Order of Australia (AO) in 2001. And I am also currently involved in a project through Sydney Uni to help improve Maternal and Child Health in Myanmar (previously Burma).”
Professor Gracey has certainly led a full life and contributed much to this country, our indigenous people and improved the lives of thousands of children the world over. He has certainly lived his life in the way of Champagnat!
Fortior Ito
Adam Hendry
President, Old Boys Union
Dr George Augustine Mende (1955)
The tragic early death from a canoeing accident on the Nepean River at Penrith on 29 May 1977 of George Mende lost to the profession a fine physician and clinician and to the community the services of a dedicated and much respected member of the medical profession. George Augustine Mende was born 8 January 1938 in Chorzow, Poland of mixed Polish and German ancestry. His family migrated to Australia in 1950 when George was twelve and he became the first ‘new Australian’ to attend Marist Brothers’ High School Parramatta, where he became, in his final year, cadet under officer and gained a fine leaving certificate pass in 1955.
George attended Sydney University from 1956 to 1961 doing his training at St Vincent’s Hospital where he became a junior resident after his graduation. He then took up a short service commission as a surgeon lieutenant in the RAN between 1963 and 1966 inclusive. During this period he saw active service aboard HMAS Stuart and Vampire in North Borneo and South Vietnam. Upon leaving the navy George became a medical registrar at Nepean District Hospital with the right of private practice and with the energy that was characteristic of him, set about the enthusiastic development of what was to become a very extensive private practice coupled with a busy schedule of clinics, ward rounds and formal teaching at Nepean and a weekly clinic at Prince of Wales Hospital.
He was the first physician resident in a rapidly expanding area which stretched from Blacktown to Bathurst and he claimed he saw more fascinating medicine in a month than city-based physicians saw in a year. His work encompassed district and cottage hospitals and geriatric units as well as the total spectrum that the referring local doctors sent him. At the time of his death, at the age of thirty-nine, he was taking part in clinical trials and preparing his findings for publication. He was also instrumental in establishing the cardiac unit at Nepean Hospital at Penrith.
George was a large, comfortable man. He jokingly gave his hobbies as medicine and it is fair to say he devoted himself to his patients and the cause of medicine. His stated goal was to lift the standard of medicine in the west and to that end he made himself ever available to the local medical community. Being genial and easy going he was a man at once warm and relaxed with his patients yet scrupulous and rigorous in the practice of what he always referred to as his art. The other love of his life was his family and few patients did not hear some of the exploits or escapades of his ‘boys’, his four young sons. As a family man, George and his wife Angela were very much part of the local community and his unexpected death stunned the people among whom they both had worked and shared their lives. George is survived by Angela and three sons. His second son Paul was killed in a horse riding accident in 1987.
Source: Royal Australian College of Physicians’ Roll


Class of 1970
Dr Patrick Farrell GP Albury
Prof. Peter Collignon ANU Canberra